Research Highlights
Go With the PVP Flow for Invitro Model of Hydrocephalus
Institutions:
Children’s Hospital of Orange County, California
Team:
Castañeyra-Ruiz, L., Lee, S., Chan, A.Y., Shah, V., Romero, B., Ledbetter, J., & Muhonen., M.
Disease Model:
Hydrocephalus
Hydrogel:
VitroGel® 3D
Catheters made from polyvinylpyrrolidone (PVP) turn out to be the most reliable in terms of not failing during the drainage of cerebrospinal fluid from children with hydrocephalus.
Catheters are soft hollow tubes that are used to drain fluid from the body. In the case of hydrocephalus, or swelling of the brain as a result of excess cerebrospinal fluid (CSF), catheters are the preferred treatments, particularly in pediatric cases. However, catheters can get clogged with cells adhering to the inside walls of the tube. In fact, this is a primary cause of failure in CSF shunts. Coating of the catheter walls is a common strategy to prevent this problem but there are many options for such coatings, some better than others.
In this paper, a team of doctors from the Children’s Hospital of Orange County compared four different catheter coating strategies to determine which would have the lowest failure rate. Success could be measured by the complete lack of cell growth in the catheter tube, or a minimal occlusion of the catheter that still allowed adequate CSF flow. The authors compared five samples of the distal ends of ventricular catheters of four types: i) barium striped; ii) barium imprinted; iii) barium and antibiotic impregnated; and iv) polyvinylpyrrolidone (PVP). Catheters are often coated or infused with barium sulfate (BaSO4) to help with imaging of catheter location.
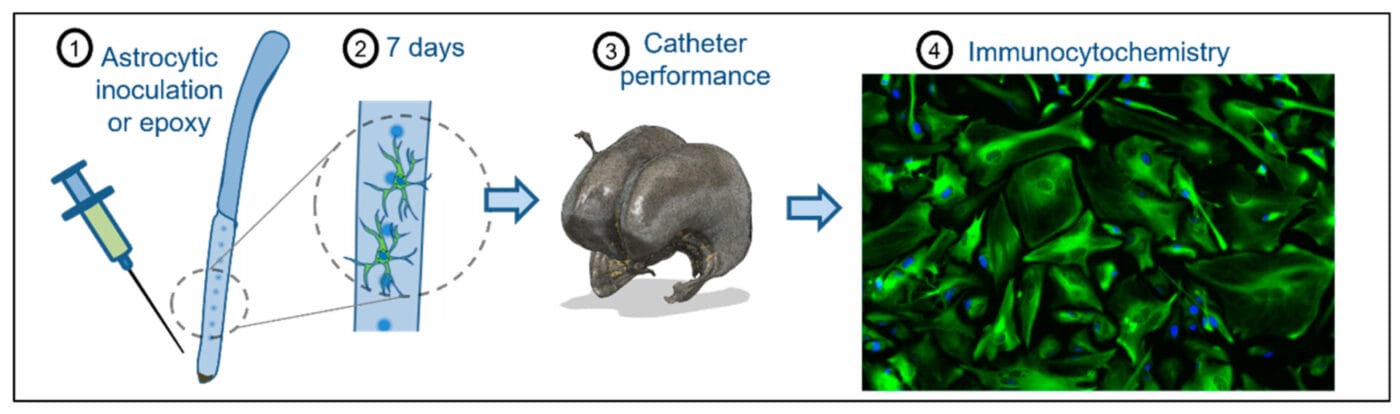
To test how well each of these catheter types was resilient to the accumulation of cells, the authors inoculated them with astrocytes, which are glial cells found in the nervous system. To grow the cells in a biotic-like environment similar to the extracellular matrix (ECM), the authors cultured them in TheWell Bioscience’s VitroGel® 3D Hydrogel Matrix. The VitroGel 3D was diluted 1:5 in Dilution Solution and the cells were mixed and grown to a final concentration of 105 cells per milliliter. After 15 minutes of this treatment, catheters were incubated at 37 °C for seven days, with media renewal every other day. Then the catheters were placed in a 3D printed hydrocephalus brain mimic, subjected to fluid flow, and imaged with fluorescent staining techniques.
Cellular adhesion and catheter flow dynamics were measured for all four catheter types and the appropriate statistics were determined across the five samples each. The authors found that the polyvinylpyrrolidone catheters were statistically superior to the other three types, both in terms of the probability of cellular adhesion and in terms of allowing flow even when a small adhesion formed. Barium-impregnated catheters performed the least well in these regards. While polyvinylpyrrolidone is unfortunately also prone to disconnect from the valve in actual patients, this study demonstrated that should this problem be fixed, there is potential for polyvinylpyrrolidone to be a material of choice for catheter manufacturing in the future for use in pediatric hydrocephalus cases.