Research Highlights
Better in 3D than 2D – Celecoxib 3D Anti-cancer Testing
Institutions:
University of Naples, Italy
Team:
Venuta, A., Nasso, R., Gisonna, A., Iuliano, R., Montesarchio, S., Acampora, V., Sepe, L., Avagliano, A., Arcone, R., Arcucci, A., and Ruocco, M.R.
Disease Model:
Melanoma
Hydrogel:
VitroGel® Hydrogel Matrix
A powerful potential anti-melanoma drug, celecoxib, is effective in 2D cultures. This new study shows that it is also the case for 3D cell cultures, which are better mimics of living tissue.
Anti-cancer drug screening is a powerful tool to assay potential chemotherapeutic strategies. Candidate compounds are mixed with cancer cell lines or tumor-derived growths in cell culture, and the subsequent growth characteristics of the cells can then be examined. The hope is that a drug can be found that retards cell growth and also proliferation into tissue mimics. Recently, it has been realized that 3D cell cultures offer a more realistic environment in which these screens can be done because they are better models to promote how cells will respond in the body.
In this study, a team of doctors from the University of Naples compared the efficacy of a potential anti-melanoma drug, celecoxib, in both 2D and 3D cell cultures. They focused on cutaneous melanoma (CM), which is a particularly lethal form of this cancer. They were interested in exploring the complete range of activity shown by celecoxib, which is a cyclooxygenase inhibitor and an NSAID that has shown some promising ability to retard CM growth under some conditions. However, there was some concern that these previous studies were all performed in 2D culture, and different behavior might be seen if celecoxib assays were performed in 3D culture.
The researchers thus tested the potential of celecoxib to restrict the abnormal growth of two melanoma cell lines in both 2D and 3D cell cultures. The scientists grew the cell lines in traditional 2D culture, both alone and in the presence of a span of concentrations of celecoxib. Cell growth properties could then be measured in time- and dose-dependent manners using cell viability assays, colony-forming assays, enzymatic expression assays, migration assays, and wound-healing assays. These all provided indications of how aggressive the cancer cells were, and how easily their growth could potentially be inhibited by the drug. The team found that the application of celecoxib between 80 and 100 μM celecoxib was reasonably effective at inhibiting cellular growth and colony formation. The effect was pronounced after about three days, and under some assays, even lower concentrations of the drug prevented colony formation.
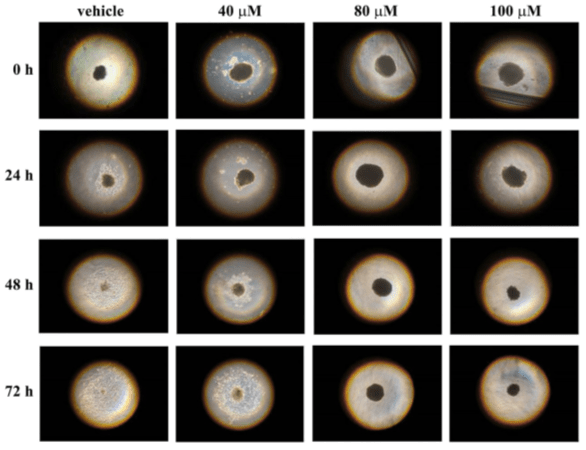
To see if these results extended to a 3D culture, the scientists generated tumor-like spheroids. Then they tested to see whether these clumps of cells could invade a hydrogel matrix, a surrogate for in vivo tissue conditions. To do this, they placed single spheroids in wells of a 96-well plate that contained 100 μL of TheWell Bioscience’s VitroGel® Hydrogel Matrix and incubated them with varying concentrations of celecoxib for three days. The results were dramatic: after treatment with 80 and 100 μM of celecoxib, the cells were not observed growing from the spheroids at all and could not invade the hydrogel. This was a clear demonstration that this dug could indeed extend a significant amount of inhibitory effect on melanoma under the 3D conditions that more closely parallel what would happen in the body than in a traditional 2D culture.
In the end, the research team concluded that celecoxib can in fact exert its toxic effects in a realistic 3D environment and that it should be a good candidate for clinical trials. These data offer hope for the eventual development of a powerful treatment for aggressive skin cancer.
Read the publication:
Related Products: